 |
| Premenstrual syndrome |
Premenstrual syndrome (PMS) refers to a compilation of over 150 symptoms that occur between ovulation and the onset of menstruation.
The symptoms include both physical symptoms, such as breast tenderness, back pain, abdominal cramps, headache, and changes in appetite; behavioral symptoms such as clumsiness, poor concentration, and sleep problems; as well as psychological symptoms of anxiety, irritability, depression, and unrest.
Severe forms of this syndrome are referred to as premenstrual dysphoric disorder (PMDD). These symptoms may be related to hormonal imbalances and emotional disorders.
 |  |
Description
Between 40-75% of all menstruating women experience symptoms that occur before or during menstruation. PMS encompasses a wide range of symptoms, some as minor as appetite change or others so severe that they may interfere with daily life.
Some women experience a beneficial increase in their sexual libido. Only 3-7% of women experience the much more severe premenstrual dysphoric disorder (PMDD). These symptoms can last 4-10 days and can have a substantial impact on a woman.
The reason some women get severe PMS while others have little or none is not understood. PMS symptoms usually begin at puberty and last until menopause.
Women more sensitive to hormonal change may experience PMS more than others. Stress is also a huge contributor and the relief of tension often lessens the other symptoms as well. Overall however, it is difficult to predict who is most at risk for PMS.
Causes and symptoms
Because PMS is restricted to the second half of a woman’s menstrual cycle, after ovulation, it is thought that hormones play a role. During a woman’s monthly menstrual cycle, which lasts from 24-35 days, hormone levels change. The hormone estrogen gradually rises during the first half of a woman’s cycle, the pre-ovulatory phase, and falls dramatically at ovulation.
After ovulation, the post-ovulatory phase, progesterone levels gradually increase until menstruation occurs. Both estrogen and progesterone are secreted by the ovaries, which are responsible for producing the eggs. The main role of these hormones is to cause thickening of the lining of the uterus (endometrium).
However, estrogen and progesterone also affect other parts of the body, including the brain. In the brain and nervous system, estrogen can affect the levels of neurotransmitters, such as serotonin. Serotonin has long been known to have an effect on emotions, as well as eating behavior.
It is thought that when estrogen levels go down during the post-ovulatory phase of the menstrual cycle, decreases in serotonin levels follow. Whether these changes in estrogen, progesterone, and serotonin are responsible for the emotional aspects of PMS is not known with certainty.
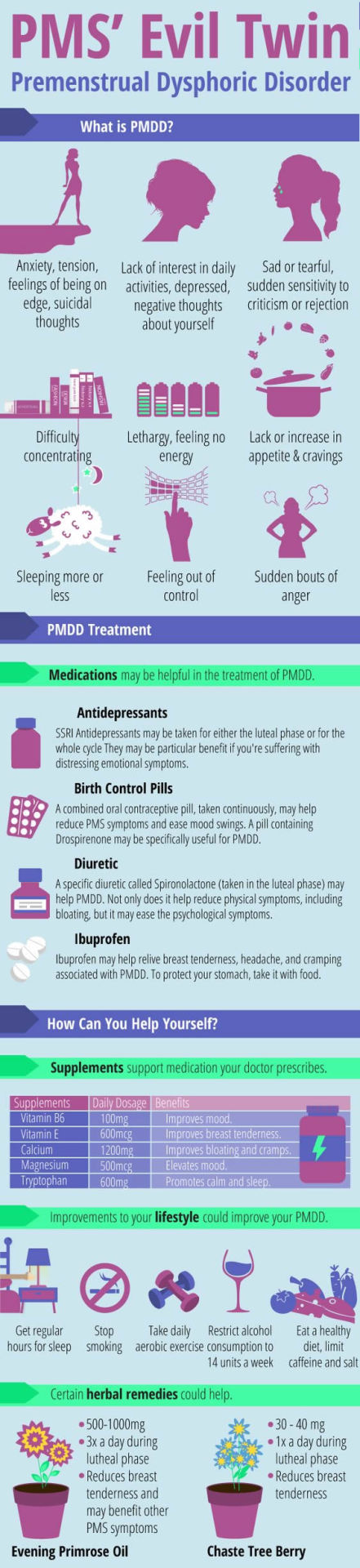 |
| Premenstrual syndrome infographic |
However, most researchers agree that the chemical transmission of signals in the brain and nervous system is in some way related to PMS. This is supported by the fact that the times following childbirth and menopause are also associated with both depression and low estrogen levels.
Nutritional deficiencies, food allergies, and hypoglycemia have been linked with PMS. A diet deficient in essential fatty acids, zinc, magnesium, and vitamin B6 may affect estrogen and progesterone production and their balance in the body.
Over 150 symptoms for PMS have been identified. These include physical, behavioral, and emotional aspects that range from mild to severe. The physical symptoms include bloating, headaches, food cravings, abdominal cramps, headaches, tension, fatigue, acne, muscle aches, and breast tenderness. Behavioral symptoms may include insomnia, lack of concentration, and clumsiness. Emotional aspects include mood swings, irritability, and depression.
Diagnosis
The best way to diagnose PMS is to review a detailed diary of a woman’s symptoms for several months. PMS is diagnosed by the presence of physical, psychological, and behavioral symptoms that are cyclic and occur in association with the premenstrual period of time.
  |
PMDD, which is far less common, was officially recognized as a disease in 1987. Its diagnosis depends on the presence of at least five symptoms related to mood that disappear within a few days of menstruation. These symptoms must interfere with normal functions and activities of the individual.
Treatment
There are many treatments for PMS and PMDD depending on the symptoms and their severity. Hypnotherapy, spiritual healing, color therapy, reflexology, Ayurvedic medicine, Chinese herbalism, acupuncture, acupressure, aromatherapy, herbal treatment, Naturopathic treatment, and homeopathy are all therapies that have been used to treat PMS.
Vitamins and minerals
Some women find relief with the use of vitamin and mineral supplements. Magnesium can reduce the fluid retention that causes bloating, while calcium may decrease both irritability and bloating. Magnesium and calcium also help relax smooth muscles, which may reduce cramping.
Recent studies indicate that calcium supplements can reduce premenstrual complaints by nearly half. Vitamin E reduces breast tenderness, nervous tension, fatigue, and insomnia. Vitamin B6 decreases fluid retention, fatigue, irritability, and mood swings. Vitamin B5 supports the adrenal glands and may help reduce fatigue.
Phytoestrogens and natural progesterone The Mexican wild yam, Dioscorea villosa, contains a substance that may be converted to progesterone in the body.
Because this substance is readily absorbed through the skin, it can be found as an ingredient in many skin creams. (Some products also have natural progesterone added to them.) Some herbalists believe that these products can have a progesterone-like effect on the body and decrease some of the symptoms of PMS.
The most important way to alter hormone levels may be by eating more phytoestrogens. These plant-derived compounds have an effect similar to estrogen in the body.
One of the richest sources of phytoestrogens is soy products, such as tofu. Additionally, many supplements can be found that contain black cohosh (Cimicifuga racemosa) or dong quai (Angelica sinensis), which are herbs high in phytoestrogens.
Red clover (Trifolium pratense), alfalfa (Medicago sativa), licorice (Glycyrrhiza glabra), hops (Humulus lupulus), and legumes are also high in phytoestrogens. Increasing the consumption of phytoestrogens is also associated with decreased risks of osteoporosis, cancer, and heart disease.
Herbal treatment
Herbal treatment has been used to treat many symptoms of PMS. Herbs to alleviate cramps include angelica root, cramp bark, kava kava, red raspberry, black haw, and rosemary. Black cohosh, peppermint, strawberry leaf, and valerian root have been used to decrease mood swings. Dandelion, couch grass, and hawthorn are effective diuretic herbs used to reduce bloating and swelling.
Burdock root and red clover are liver cleansing herbs that can be useful in eliminating excess estrogen from the system. Herbs to balance hormones include blessed thistle, dong quai, false unicorn root, fennel seed, sarsparilla root, and squaw vine. Feverfew may be effective for migraine headaches.
Many herbs may be beneficial as a natural antidepressant. St. John’s wort (Hypericum perforatum) has stood up to scientific trials as an effective antidepressant.
As with the standard antidepressants, however, it must be taken continuously and does not show an effect until used for four to six weeks. There are also herbs, such as skullcap (Scutellaria lateriflora) and kava kava (Piper methysticum), that can relieve the anxiety and irritability that often accompany depression.
An advantage of these herbs is that they can be taken when symptoms occur rather than continually. Chasteberry tree (Vitex agnus-castus), in addition to helping rebalance estrogen and progesterone in the body, may also relieve the anxiety and depression associated with PMS.
Aromatherapy
Aromatherapy oils can be a useful adjunct treatment for PMS. Lavender oil reduces headaches, cramps, and painful breasts. Chamomile and sandal-wood oils may be used to relieve stress and tension. Premenstrual fatigue may be remedied by geranium, bergamot, and rosemary oils.
Homeopathy
A number of homeopathic remedies may be applied in the treatment of PMS, depending upon the individual’s symptoms. Natrum muriaticum may be the appropriate remedy when irritability, lack of self-confidence, depression, anxiety, and headaches are present.
Sepia may be given when PMS is accompanied by stress, weepiness, and to calm nerves. Symptoms of indifference, panic attacks, anger, tension, hair loss, sugar cravings, and a reduced sex drive may indicate that Kali carbonicum may be the appropriate remedy.
Allopathic treatment
Allopathic treatments available include over-the-counter anti-inflammatory drugs such as ibuprofen or acetominophen, antidepressant drugs, hormone treatment, or (only in extreme cases) surgery to remove the ovaries.
Anti-inflammatory drugs are useful in reducing headaches, muscle aches, and cramping. One recommendation is to begin taking the anti-inflammatory one to two days before the onset of cramps. Doing so will block the cramp-causing hormones, prostaglandins, and may prevent any nausea, vomiting, and diarrhea associated with PMS.
Hormone treatment usually involves oral contraceptives. This treatment used to prevent ovulation and the changes in hormones that accompany ovulation. Recent studies, however, indicate that hormone treatment has little effect over placebo.
Antidepressants
Antidepressants prescribed for PMS include sertraline (Zoloft), fluoxetine (Prozac), and paroxetine (Paxil). They are termed selective serotonin reuptake inhibitors (SSRIs) and act by indirectly increasing the brain serotonin levels, thus stabilizing emotions.
Some doctors prescribe antidepressant treatment for PMS throughout the cycle, while others direct patients to take the drug only during the latter half of the cycle. Antidepressants should be avoided by women wanting to become pregnant. Side effects of sertraline were found to include nausea, diarrhea, and decreased libido.
Expected results
The prognosis for women with both PMS and PMDD is good. Most women experience relief from symptoms when treated.
Prevention
Maintaining a good diet, one low in sugars, salt, fats, alcohol, and caffeine, and high in phytoestrogens and complex carbohydrates, may prevent some of the symptoms of PMS.
Consumption of more complex carbohydrates may relieve PMS symptoms since carbohydrates drop seratonin levels as they raise insulin levels. For instance, two cups of cereal or a cup of pasta has enough carbohydrate to effectively increase serotonin levels. Carbohydrates also provide steady levels of blood sugar and act to stabilize one’s mood.
One recommendation is to eat 100 calories of complex carbohydrates every three hours beginning one week before menstruation. Complex carbohydrates include whole wheat bread and pasta, brown rice, and whole grain foods. Caution should be taken due to the fact that a high carbohydrate diet causes water retention, which in turn is a symptom of PMS.
Women should try to exercise three times a week, keep in generally good health, and maintain a positive self image. Because PMS is often associated with stress, avoidance of stress or developing better means to deal with stress can be important. Relaxation techniques, meditation, and yoga practice can aid in stress reduction.
